-
-
Featured Care Areas

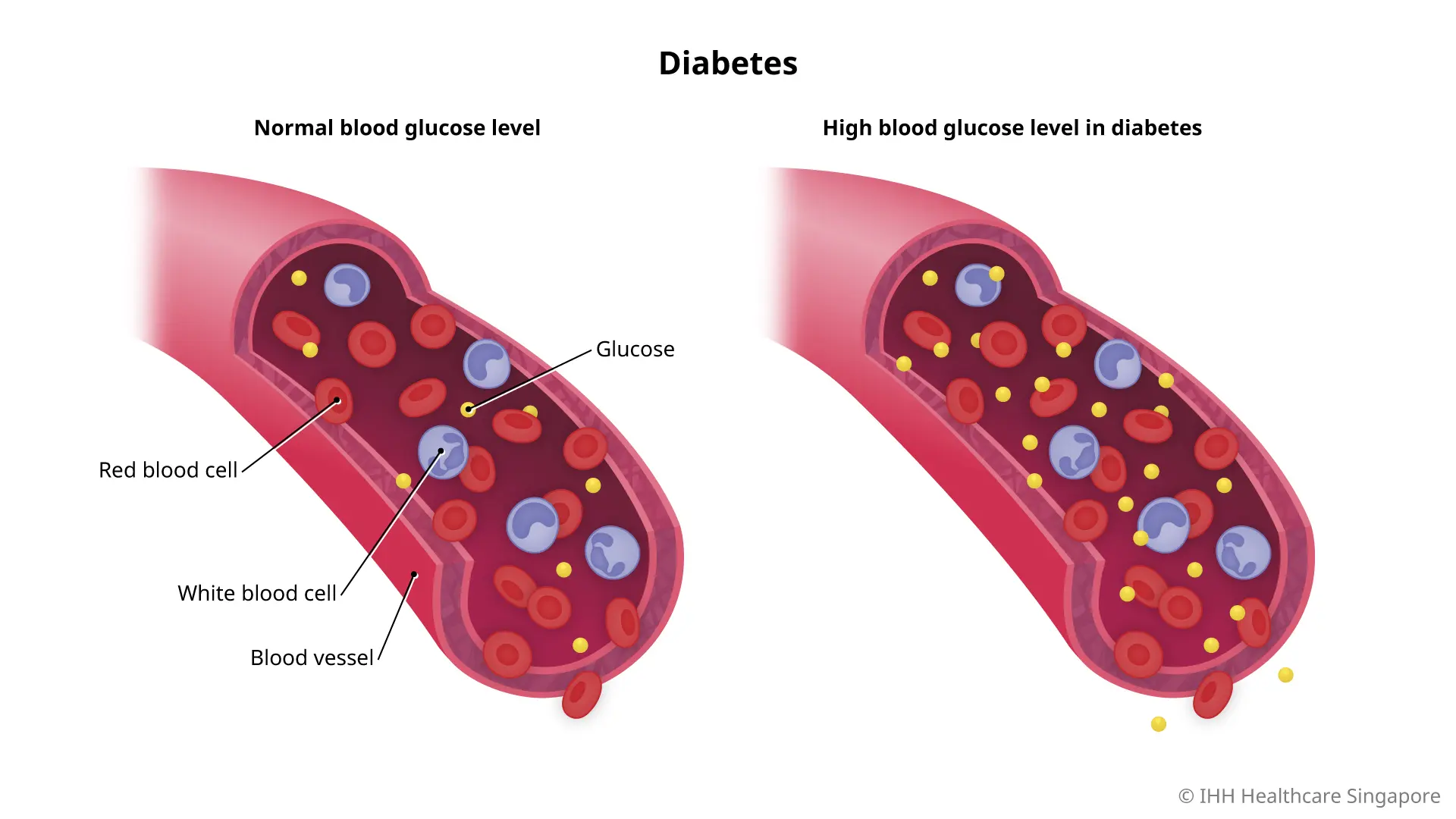
Diabetes
What is diabetes?
Diabetes mellitus, commonly referred to as diabetes, is a chronic condition characterised by elevated levels of glucose in the blood. It arises from issues with insulin production, insulin action, or both. Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels.
Types of diabetes
There are 3 main types of diabetes:
- Type 1 diabetes: An autoimmune condition where the body's immune system attacks and destroys the insulin-producing cells in the pancreas
- Type 2 diabetes: The most common form, associated with the body's ineffective use of insulin, often due to lifestyle factors and genetics
- Gestational diabetes: Occurs during pregnancy and usually disappears after giving birth, though it increases the risk of developing type 2 diabetes later in life
What are the symptoms of diabetes?
Symptoms of diabetes can develop rapidly in type 1 diabetes but may be gradual or even absent in type 2 diabetes. Common symptoms include:
- Increased thirst and frequent urination
- Extreme hunger
- Unexplained weight loss (more common in type 1)
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Tingling or numbness in the hands or feet (type 2)
What causes diabetes?
The exact cause of diabetes varies by type:
- Type 1 diabetes is primarily caused by an autoimmune reaction that destroys the insulin-producing beta cells of the pancreas.
- Type 2 diabetes results from a combination of genetics and lifestyle factors, such as poor diet, insufficient physical activity, and obesity.
- Gestational diabetes is caused by hormonal changes during pregnancy that make the body's cells less responsive to insulin.
Who is more at risk of developing type 2 diabetes?
Certain factors increase the risk of developing diabetes, particularly the most common type 2 diabetes. Here are the key risk factors:
- Age: The risk increases as you get older, particularly after age 45. However, type 2 diabetes is also increasingly being seen in younger populations, including adolescents.
- Weight: Being overweight or obese is a primary risk factor for type 2 diabetes. Excess body fat, especially if stored around the abdomen, can increase the body’s resistance to the hormone insulin.
- Family history: Having a parent or sibling with diabetes significantly increases the risk.
- Ethnicity: People of certain ethnicities, including African, Caribbean, South Asian, Hispanic, and Native American descent, are more likely to develop type 2 diabetes.
- Physical inactivity: A sedentary lifestyle contributes to obesity and type 2 diabetes. Regular physical activity helps control weight, uses up glucose as energy, and makes cells more sensitive to insulin.
- Gestational diabetes: Women who develop gestational diabetes during pregnancy are more likely to develop type 2 diabetes later in life.
- Polycystic ovary syndrome (PCOS): Women with PCOS have a higher risk of developing type 2 diabetes.
- High blood pressure and abnormal cholesterol levels: These conditions often accompany type 2 diabetes and can increase the risk further.
- Impaired glucose tolerance or impaired fasting glycaemia: These are intermediate conditions between normal glucose homeostasis and diabetes, also known as prediabetes, significantly raising the risk of progressing to type 2 diabetes.
What are the complications and related diseases of diabetes?
Long-term complications of diabetes develop gradually and can become life-threatening:
- Cardiovascular diseases, including heart attack, stroke, and hypertension
- Nerve damage
- Kidney damage
- Eye damage that can lead to blindness
- Foot damage, potentially leading to ulcers, infections, and possible amputation
- Skin conditions, including bacterial and fungal infections
- Hearing impairment
- Alzheimer's disease (more likely in type 2 diabetes)
Individuals with diabetes have an increased risk of developing kidney failure, also known as diabetic nephropathy. This condition is one of the most serious complications of diabetes, occurring as a result of long-term damage to the small blood vessels in the kidneys. Over time, the kidneys' ability to filter waste products from the blood deteriorates, which can lead to kidney failure.
Regular monitoring of kidney function through blood and urine tests is recommended for those with diabetes to detect any signs of deterioration early, allowing for timely intervention to prevent or delay the progression to kidney failure.
How do you prevent diabetes?
Prevention of type 2 diabetes is possible through lifestyle changes:
- Maintain a healthy weight
- Engage in regular physical activity
- Eat a balanced diet rich in fruits, vegetables, and whole grains
- Avoid excessive sugar and saturated fats
- Regularly monitor your blood glucose levels if at risk
Type 1 diabetes cannot be prevented due to its autoimmune nature.
This coverage checker is brought to you by Health Insured, an online resource that helps you understand your health coverage in Singapore.
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6377 3737
For appointment bookings, please WhatsApp
+65 8111 3777